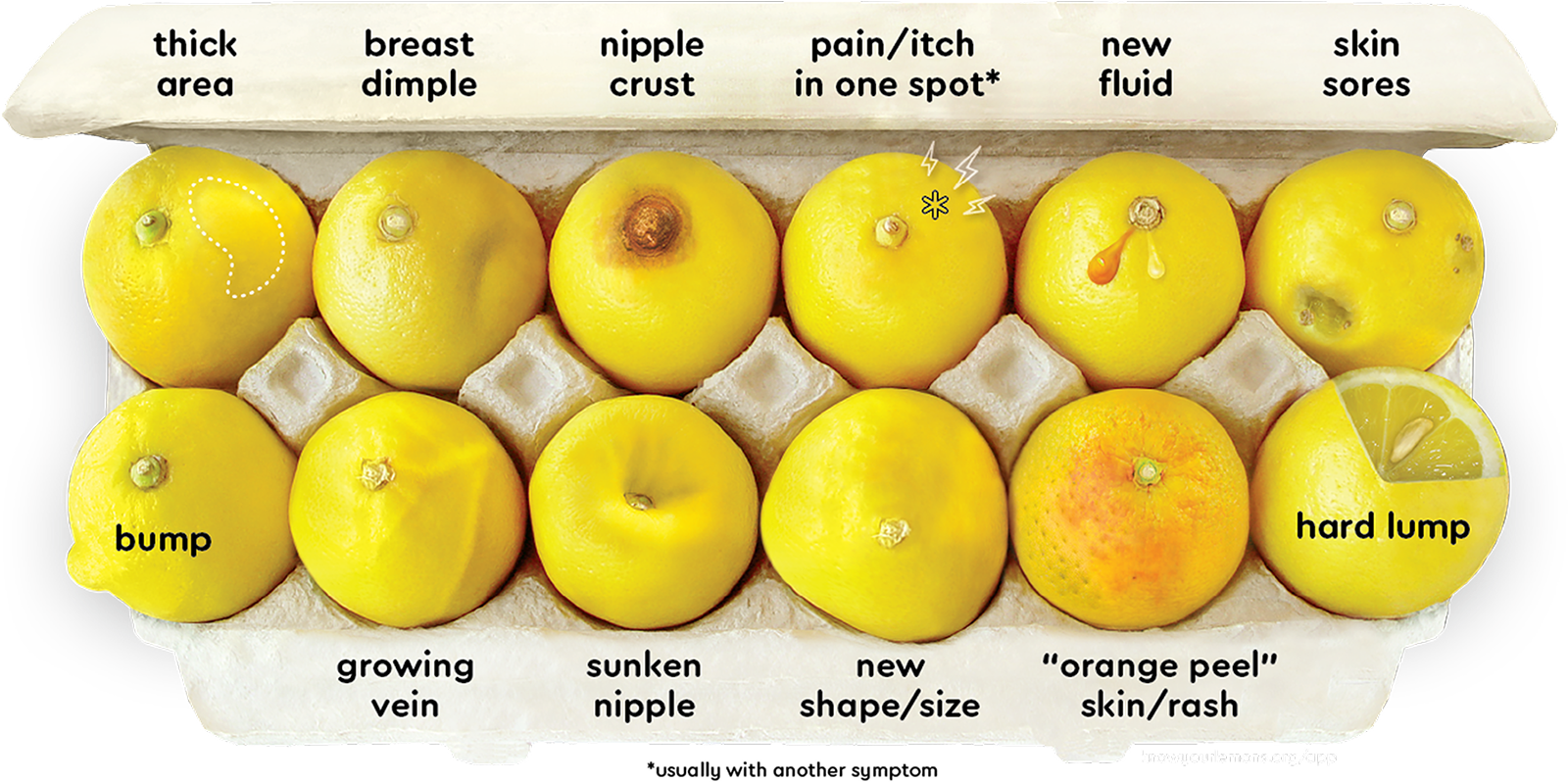
12 Symptoms of Breast Cancer: What it can look and feel like
For warning signs of breast cancer, there is more than just a lump. Learn about each symptom and get the free app to explore your breast cancer risk factors and get your risk score to get a custom screening plan, learn how to do a proper self-exam, and schedule your mammogram right on the app.
-
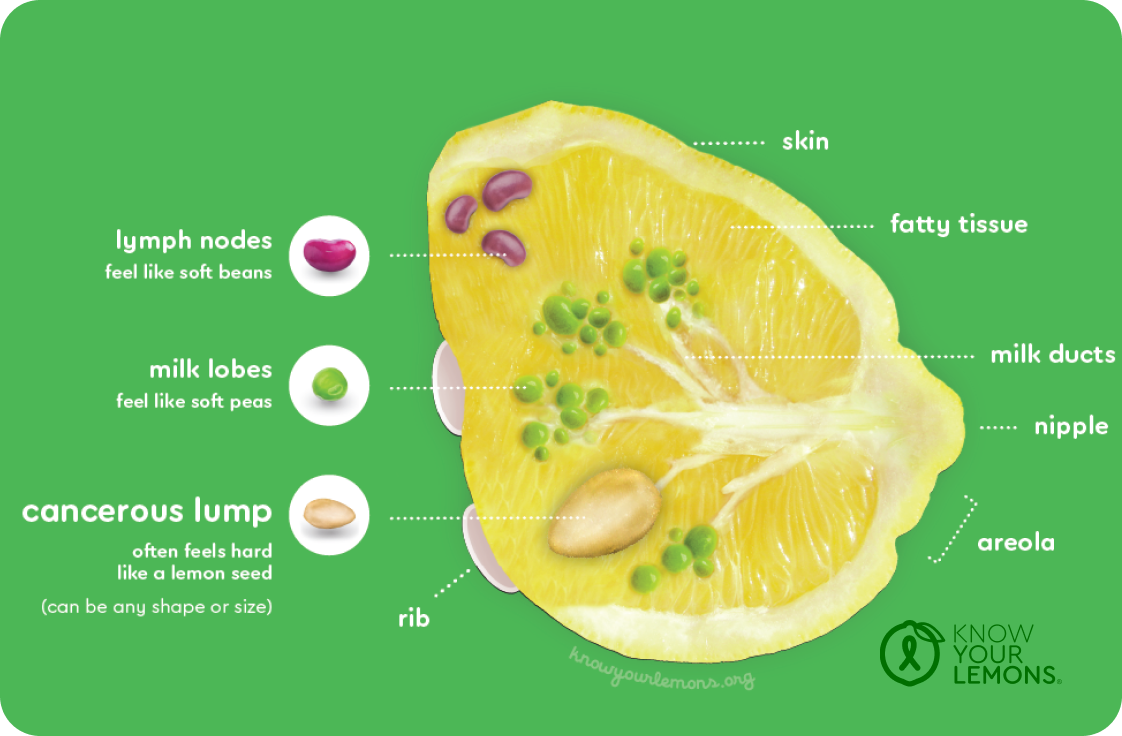
A lump is not always easy to feel
The most common sign of breast cancer, a lump often feels hard (like a lemon seed). It can be any shape or size, but is not always easy to feel. Mammograms can detect a lump long before it can be felt. If you notice a hard lump, or any change, that doesn’t come and go with your menstrual cycle, don’t ignore it. The sooner breast cancer is found, the more easily it can be treated.
-
Don’t confuse thickness with breast density
You may notice that a part of your breast feels different from the rest, being less squishy and more dense. This can be a normal part of menstruation or breast feeding, but a thickening in your breast that doesn’t go away or gets worse could be a sign of breast cancer.
-
Dimples that don’t go away can be a sign of breast cancer
Dimples are caused when a tumor (lump) deep in the breast pulls the skin inward, causing it to indent. Sometimes this lump can be felt, sometimes it can’t. A dimple can be more easily seen when lifting your arms above your head to see if the whole breast skin moves with you. Having a light source directly overhead can help cast shadows to show indents more clearly.
-
Separating a normal skin condition from a troublesome symptom
Crust on the nipple can be a harmless skin condition, like eczema, or is a common problem with breastfeeding. But if skin remedies don’t fix the problem, it could be a sign of breast cancer called Paget’s Disease. This when cancer cells spread inside the breast and live in the nipple, creating a scab-like red or white crusted surface that can be sore and doesn’t go away.
-
Pain or itching is a common issue with breasts but sometimes it’s a concern
Breast pain is very common and most often harmless, usually related to hormones and menstrual cycle changes. However, if the pain is in one spot, persistent (doesn't change with your menstrual cycle) or gets worse, it should be checked out like any unexplained pain anywhere in your body. Pain is also more suspicious if another breast cancer symptom is present.
Like pain, itching in the breast is usually not a symptom of breast cancer. However, sometimes cancer can interfere with nerve endings, which causes an itching sensation that doesn't go away—such as with Inflammatory Breast Cancer (IBC).
-
Fluid from the nipple outside of breast feeding isn’t normal
Discharge from the nipple is common and is harmless (benign) most of the time. It is usually related to developing breasts, infection, cysts, pregnancy, or breastfeeding. However, if fluid is leaking from the breast outside of these changes, it is something that should be checked out, especially if it is clear or contains blood.
-
Usually an advanced sign of breast cancer
Breast cancer can sometimes build up to the point that it breaks down the skin of the breast to form an open wound. Infection may cause a bad smell and/or leakage. This is usually accompanied by an obvious hard lump. This is an advanced sign of the disease, meaning it has been present for some time.
-
If it’s new and stays around, it should be checked out
Sometimes a cancerous lump is on the surface of the breast. But not all lumps and bumps are cancer. Many are cysts (fluid collections) or harmless lumps made of various tissue (fibroadenomas). Sometimes an injury can lead to a lump known as fat necrosis. This is scar tissue that can form when the body naturally repairs the damaged fatty breast tissue.
-
Keep an eye on your veins
Enlarged veins is one of the rarer symptoms of breast cancer and are often seen with normal skin changes. Newly appearing blood vessels or veins are more often connected to weight gain, breastfeeding and Mondor’s disease and are not usually a sign of cancer. However, if veins become more pronounced outside of these changes, on the breast or near the collarbone (and sometimes accompanied by a swollen arm), this could be a sign of a breast cancer tumor drawing more blood to itself and the vein swelling in size to allow for additional blood flow.
-
Watch for changes in nipple direction
Retracted nipples can be a normal shape of the breast, from when the breast was first developed. If you notice your nipple sinking, flattening or turning, it could be a sign of a new breast cancer tumor forming underneath, pulling the nipple toward it as it grows.
-
Be familiar with the normal shape and size of your breasts
It’s common for one breast to be different in size and shape from the other. Breastfeeding can also cause changes in size or shape as a result of milk production. But if one breast changes size, flattens, swells or droops unexpectedly — and doesn’t seem to be connected to your menstruation cycle — this could be a sign of breast cancer.
-
Skin changes could be a simple skin issue or something more suspicious
If a breast changes color (reddish or dark), texture (rash or dimpled skin) or feels warm, it is often a sign of infection, developing breasts, breastfeeding or eczema. If antibiotics or other treatments don’t resolve the issue, it may be a symptom of Inflammatory Breast Cancer. This symptom is difficult to see on a mammogram because it does not form an obvious lump.
Once you know what your “normal” is, it’s easier to spot a change. Knowing the 12 signs of breast cancer can help you know what to look and feel for. Use the app to explore and document your normal—and perform guided self-exams each month. But remember, self-exam is only one part of early detection. Screening finds breast cancer early—often before symptoms appear. The Know Your Lemons app helps you know your risk score and build the right screening plan for you.
Prevention and Early Detection:
Self-Exams & Mammograms
Every 14 seconds someone around the world is told, "You have breast cancer."
Early detection can save their lives.
Perform regular self-exams with confidence. The best time to self-exam is a few days after the end of your period when you are least tender and swollen. It’s easy to forget to do it, but our app sends reminders.
When it comes to feeling confident, that starts with knowing what lumps are normal and which are a concern. There’s more to know than just feeling for a lump too—and our award-winning app will teach you with our fun audio guides and step-by-step instructions to know what to do if you notice a change.
A mammogram can find a cancerous lump before it can be felt.
When to start them and how often to do them depends on your individual risk factors. Current guidance suggests starting mammograms at age 40 in most countries, but your family history and other factors might suggest a different screening plan. Download our app for your personalized screening recommendation by calculating your risk score. A customized screening plan for you to share with your doctor will be tailored to you.
Know Your Risk
Everyone is at risk of developing breast cancer — some with a higher risk than others. These risks come from things we can and cannot control. Knowing what your risk factors are, how they influence screening plans, and how you can take charge of your health is your key to early detection and prevention.
Personal Health Factors
-
The higher your age, the higher your risk for breast cancer. The longer you are exposed to estrogen, the longer you’ve been exposed to increased risk.
-
Periods increase the amount of estrogen in the body. The more periods you’ve had, the more exposure you’ve had. The risk of breast cancer is lower for women who are pregnant before age 35. This is because breast cells are copied rapidly during pregnancy as part of breastfeeding changes. The older the cells, the greater the chance of mutation, which may create more bad copies, leading to a slightly increased risk for breast cancer.
-
Not all hormone pills or birth control pills increase your risk for breast cancer, but some can. Talk to your doctor about whether the medications you are taking have a breast cancer risk associated with them.
Lifestyle Factors
-
Consuming alcohol, as well as smoking cigarettes, increases your risk for breast cancer.
-
Did you know that fat cells make and store estrogen? Your risk of breast cancer increases if you are overweight, especially after menopause. Maintaining a healthy weight can reduce your risk. Losing weight also means you lose the extra estrogen along with it.
-
Not exercising regularly, or being sedentary for long periods of time can also contribute to your risk for breast cancer. Many studies conducted over the past 20 years have shown that an increase in physical activity is linked to lower breast cancer risk. Physical activity regulates hormones, including estrogen and insulin which can fuel breast cancer growth. The American Cancer Society recommends at least 150 minutes of moderate-intensity exercise each week (about 20 minutes a day) and 75 minutes of vigorous intensity each week (about 9 minutes a day).
Genetic Factors
-
Certain breast conditions may increase your risk for breast cancer. These include complex fibroadenomas, certain types of cysts, atypical hyperplasia, papillomas, and lobular carcinoma in situ (LCIS) (BRCF, 2022). Additional screening may be recommended for these breast conditions.
-
Half of women over 40 have dense breasts, which increases your risk for breast cancer. Breast density is not something you can feel; it can only be determined through a mammogram. You are more likely to have dense breasts if you are young, thin, Asian, or Black. Talk to your doctor about additional screening options.
-
A family history of breast cancer increases your risk because you may share a genetic mutation. Talk to your doctor about genetic testing – if available – if it’s a concern in your family.
Although a family history of breast cancer can increase your risk, it's important to remember that about 85% of people with breast cancer do not have a family history of breast cancer so everyone is at risk (Breastcancer.org, 2024).